Hundreds of Topics for Every Role
You don’t have to choose between best-in-class clinical and soft skills training.
Your atdove.org subscription offers content for every member of your team—from the front desk to the O.R.
Surgery + Anesthesia
Build confidence in surgical prep and methods with step-by-step procedurals.
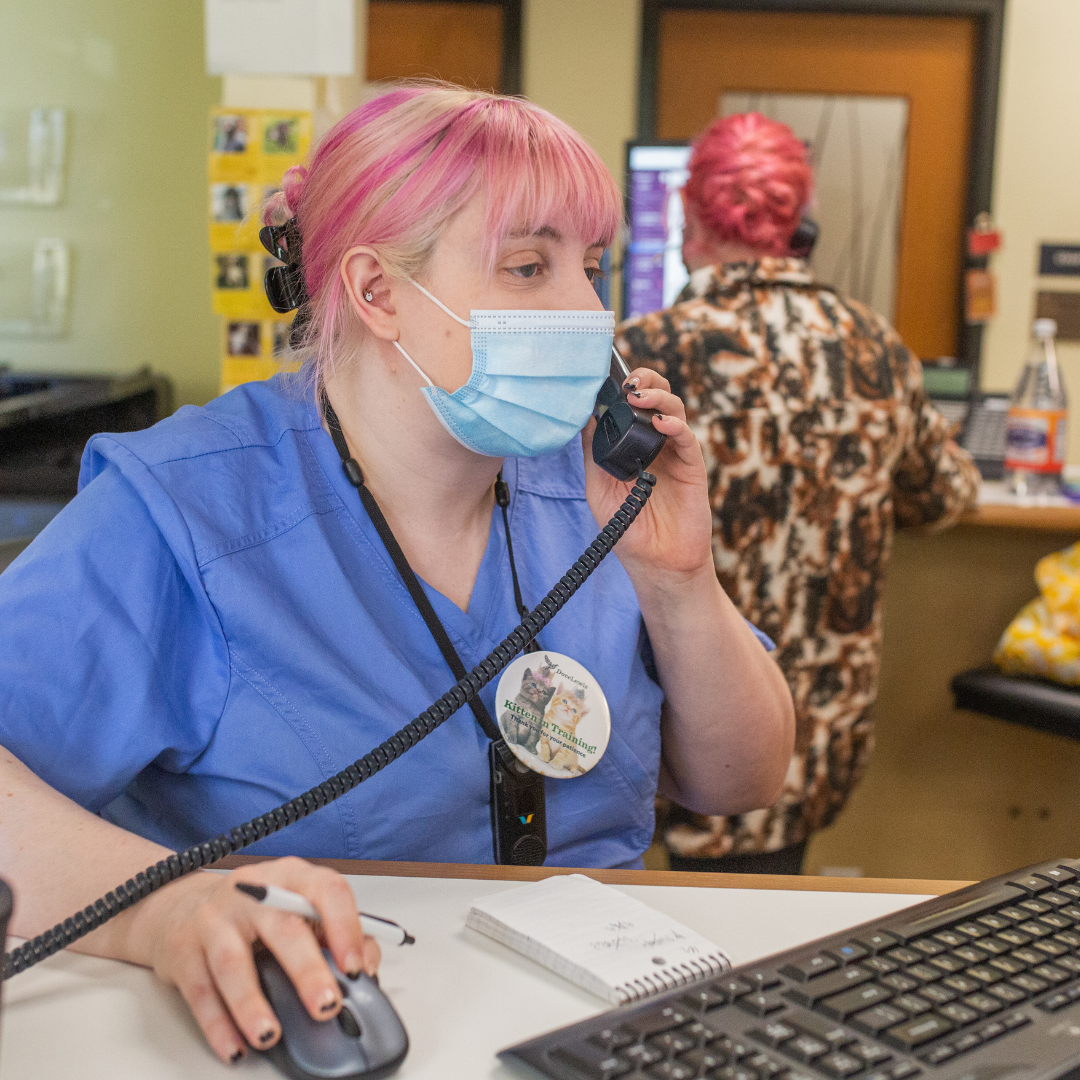
Client Communication
Honing phone and in-person communication for an improved client experience.
The Art of Triage
Implement an efficient triage process for emergent patients.
Technician Basics
Standardize key skills like restraint, handling, and IV catheter placement.
Medical Math
Practice conversions, calculating CRI, and other everyday skills.
Interpreting Diagnostics
Review standard diagnostic tools and tests like PCV and cytology.
New Content Uploaded Every Week
Duck Wing Amputation
Kelly Flaminio, DVM, discusses the wing amputation surgery and postoperative care for a duck that suffered a traumatic injury.
Well-being Considerations for Career Longevity
In collaboration with the Humane Society Veterinary Medical Association, Debrah Lee, LCSW, provides resources and guidance for those working in veterinary medicine.
A Variety of Ways to Learn
Tools for Managers
We get it—implementing training and onboarding for new hires takes time. Our manager tools make it easier to standardize care at your clinic. Our tools include:
What Our Users Say
Ready to get started?
Try it free for 7 days. Subscriptions start at just $59.99 a month for up to 50 team members!
We offer both annual and flexible month-to-month options to meet your needs.